What we carry with us
Julie Egan
Nearly all my ancestors migrated from Ireland in the 1860s. The O’Connors, O’Rourkes, Careys, and Egans decided that Australia offered them a better future than post-famine Ireland. Between 1845 and 1852, failure of the potato crops due to infestation by potato blight mold led to death by starvation and disease of approximately one million people, and mass evictions of landholders unable to pay rent. Lured by the promise of a vast new country, they probably travelled to Liverpool, there to embark on a perilous weeks-long journey to an unknown country and an unknown future. For many, this would have been the first time they had left their villages or towns.
I carry this history in my body. My fair skin is the legacy of the thousands of years of evolution that allowed my shivering ancestors to make the most of the feeble northern sun and produce vitamin D. The influences of the mountains and mist, the peat bogs and the rocky coastlines, are in my DNA. I carry a copy of the gene for haemachromatosis, known as the Celtic curse because of its prevalence in people of Irish or Northern European descent. Different forms of this disease cause the body to accumulate more iron than needed, which can lead to organ damage. A variant of the gene has been identified in the remains of a woman who lived about 5000 years ago in the north of Ireland. My red hair is linked to the melanocortin-1 receptor (MC1R) gene.
On my first visit to Ireland in my 20s, I hitchhiked along a lonely road south of Dublin. A car passed occasionally. My backpack was too heavy and I would rest on one of the low stone fences bordering a field. Yet I felt at home. Was it just a romantic idea, born of growing up with a father who sang Irish songs and told stories about leprechauns and banshees, of St Patrick driving the snakes out of Ireland, of famines and the Easter Rising? But the people I met looked like me. A motorist who picked me up commented that ‘the Egan girls always had red hair’. Perhaps for the first time my body was in the environment it had evolved to fit.
Maybe I have also inherited more subtle indicators of my ancestors’ experiences. The environmental can modify our genetic material without altering our DNA code, and some of these epigenetic changes can be transmitted from one generation to the next. For example, in the Hunger Winter of 1944–1945, the Nazis blocked food supplies to the western provinces of The Netherlands. Locals resorted to eating tulip bulbs and nettles, and more than 20,000 people died. Churches were used as temporary morgues. Not surprisingly, being in utero during a time of famine wasn’t the best start to life, and babies born during that time were often underweight and had higher rates of diabetes, obesity, and schizophrenia in later life. The real surprise came in the next generation, who were also affected: grandchildren of pregnant women carrying female babies during the Hunger Winter were also smaller at birth and had poorer health. It seemed that famine conditions had led to inheritable modification of certain genes.
Do I carry the marks of the Irish famine, the Great Hunger, in my DNA? Some of my ancestors would certainly have been born during that time of death and devastation. Does my DNA now also carry the marks of living here, in Australia? Do I now ‘belong’ here more than those of my ancestors who arrived in the 1860s? Do I carry the marks of this landscape?
My DNA has made some migrations alone. I have no doubt left behind skin flakes and hairs in all the places I have lived and travelled. I imagine a world map with a smattering of icons, perhaps tiny little helices, showing where my DNA might be found. All probably degraded and mixed with DNA from other humans, other animals, plants. Perhaps my DNA can still be found in freezers in hospitals and laboratories. Countless blood samples, skin, bone marrow and colon biopsies, my spleen, tonsils, appendix, and a couple of skin cancers have been removed and examined to treat or diagnose events on my body’s journey through life.
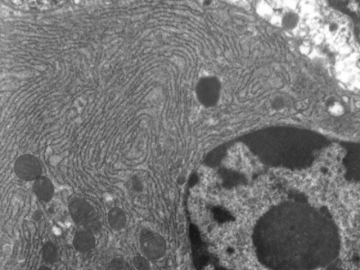
Closer to home is the DNA in my two children. The reshuffling that occurred when their father’s DNA and mine combined, means that they share enough of my DNA to be identified as my children, but they are not clones. But research has now shown that my children and my grandchildren and I share much more than some DNA sequences. During pregnancy the placenta sheds cells into the mother’s bloodstream. These cells degrade, releasing DNA which is usually identical to that of the foetus. This transfer of intact living foetal cells occurs in all pregnancies, starting in the fourth or fifth week after fertilisation and continues throughout pregnancy. The foetal cells can be detected in the mother’s blood for up to thirty days after birth and can persist in organs such as skin, bone marrow, brain, lungs and liver for decades. Foetal cells from previous pregnancies can also persist. While such cell transfer has been known for decades, it is only recently that the technology has developed to allow non-invasive testing. When I was pregnant as a geriatric mother (obstetric terms can be discouraging), I underwent chorion villus sampling to screen for abnormalities in the baby. This involved taking samples of the placenta either transvaginally or through the abdomen wall at around 10–12 weeks. Painful, invasive and with a risk of miscarriage. Now all my daughter and daughter-in-law need to do is provide a blood sample.
Nearly every woman who has been pregnant is therefore a chimera, an organism made up of different populations of genetically distinct cells. Greek mythology is replete with such creatures: Pegasus, the Gorgons, centaurs, griffins. Nothing so dramatic for mothers; here we are talking about microchimerism, with one population of cells at a very low level.
Transfer of cells between the foetus and the mother is not just one-way. Cells also migrate from the mother to the foetus during pregnancy, and can be found in newborns in the skin, liver, spleen and thyroid. These cells can persist well into adult life. Cells in the mother’s breast milk may also enter through the baby’s gut lining, particularly via colostrum, the milk produced during the first few days. My genome, my intact DNA bearing the marks of my history and those of my distant Irish ancestors, may persist in my children.
Grandmaternal cells have been found in cord blood but it is not known whether these also persist into adult life. While it is a truism to speak of achieving immortality by having children, it therefore seems that it may be true in a very physical sense. When I embrace my new hours-old grandchild, I am holding someone who carries parts of me and my child and perhaps my distant ancestors.
Half a globe and a century and a half away, I imagine one of my ancestors standing on a beach in Ireland, taking a final walk before she began her journey to a new life in Australia. I imagine the cold grey-green sea lapping around her feet and the blue veins standing out on her white skin. The memories of that cold water still run in my blood and in my children and my grandchildren. Maybe in my chimeric body she also lives on.
The science inspiring the piece
'Grandmaternal cells in cord blood' via eBioMedicine
'Maternal-fetal cellular trafficking: clinical implications and consequences' via National Library of Medicine